Preventive Approach in Non-Alcoholic Fatty Liver Disease
DOI:
https://doi.org/10.36790/epistemus.v16i32.185Keywords:
OBESITY, PUBLIC HEALT, BIOACTIVE COMPOUNDS, NON-ALCOHOLIC FATTY LIVER, PREVENTIVE APPROACHAbstract
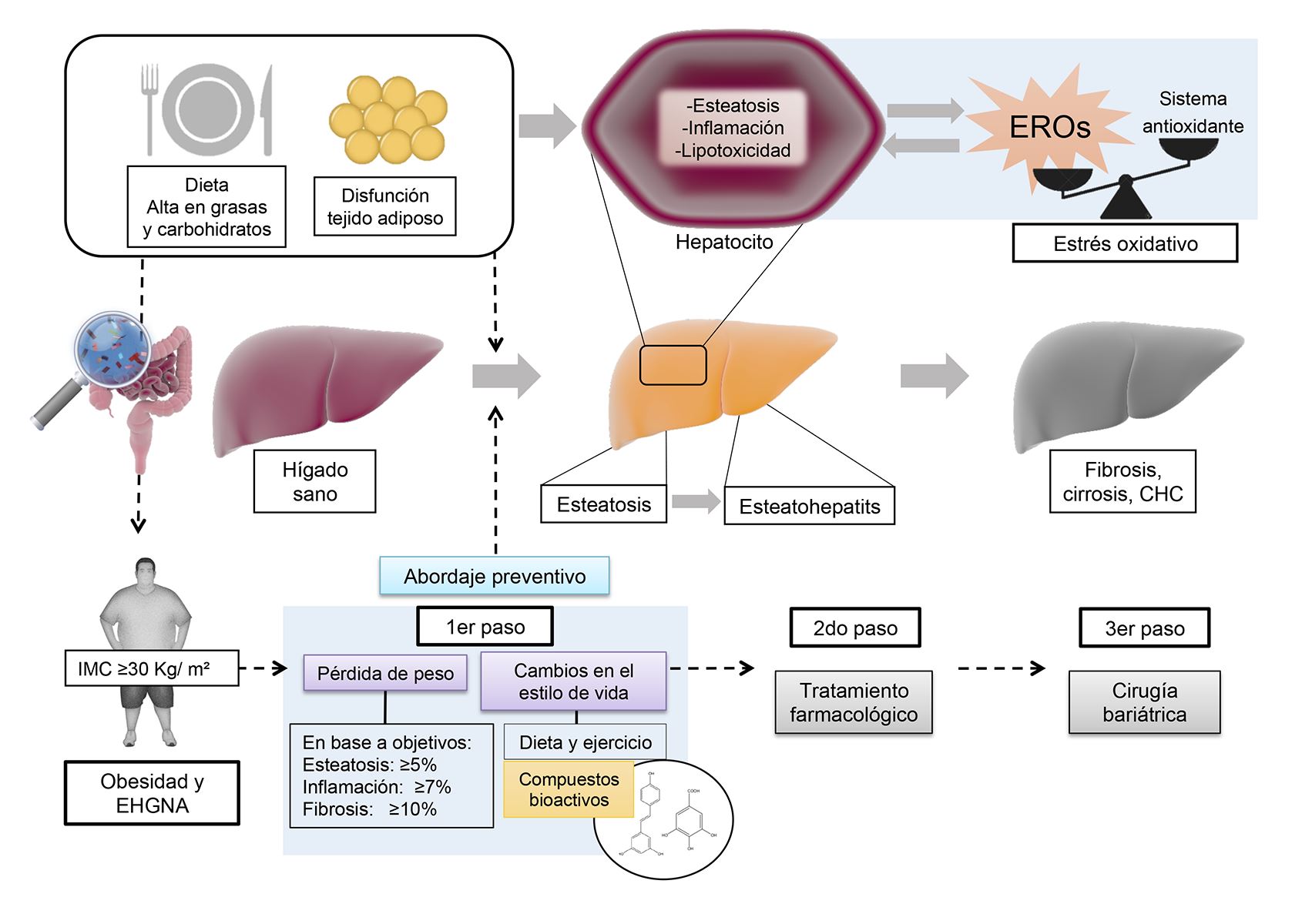
Obesity is currently a worldwide public health problem. It is characterized by its negative impact on multiple organs, including the liver, through the development of diseases such as non-alcoholic fatty liver disease (NAFLD), which can promote the development of hepatocellular carcinoma. This review discusses the association between obesity and the development of NAFLD, emphasizing on the importance of a preventive and interventional approach during the early stages of the disease, as well as the potential effect of some dietary bioactive compounds. In this regard, it is advisable to focus the intervention on improving BMI, through a program of physical activity, nutritional and health education, and changes in dietary patterns. The inclusion of foods rich in bioactive compounds, such as phenolic compounds, fiber and vitamins can provide an antioxidant, anti-inflammatory and anti-obesogenic effect that could hinder the progression of NAFLD and other comorbidities and complication.
Downloads
References
Y. C. Chooi, C. Ding, and F. Magkos, “The epidemiology of obesity,” Metabolism, vol. 92, pp. 6–10, Mar. 2019. DOI: https://doi.org/10.1016/j.metabol.2018.09.005
NCD Risk Factor Collaboration, “Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants,” Lancet, vol. 387, no. 10026, pp. 1377–1396, Apr. 2016. DOI: https://doi.org/10.1016/S0140-6736(16)30054-X
R.-D. J. Shamah-Levy T, Romero-Martínez M, Barrientos-Gutiérrez T, Cuevas-Nasu L, Bautista-Arredondo S, Colchero MA, GaonaPineda EB, Lazcano-Ponce E, Martínez-Barnetche J, Alpuche-Arana C, “Encuesta Nacional de Salud y Nutrición 2020 sobre Covid-19. Resultados nacionales.,” Cuernavaca, México, 2021. [Online]. Available: https://ensanut.insp.mx/encuestas/ensanutcontinua2020/doctos/informes/ensanutCovid19ResultadosNacionales.pdf. DOI: https://doi.org/10.21149/12580
NCD Countdown 2030 collaborators, “NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4.,” Lancet (London, England), vol. 392, no. 10152, pp. 1072–1088, 2018. DOI: https://doi.org/10.1016/S0140-6736(18)31992-5
M. Aceves-Martins, E. Llauradó, L. Tarro, R. Solà, and M. Giralt, “Obesity-promoting factors in Mexican children and adolescents: challenges and opportunities.,” Glob. Health Action, vol. 9, p. 29625, 2016. DOI: https://doi.org/10.3402/gha.v9.29625
N. Chalasani et al., “The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases.,” Hepatology, vol. 67, no. 1, pp. 328–357, 2018. DOI: https://doi.org/10.1002/hep.29367
Z. Younossi et al., “Global Perspectives on Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis.,” Hepatology, vol. 69, no. 6, pp. 2672–2682, 2019. DOI: https://doi.org/10.1002/hep.30251
M. M. Betancourt-Garcia, A. Arguelles, J. Montes, A. Hernandez, M. Singh, and R. A. Forse, “Pediatric Nonalcoholic Fatty Liver Disease: the Rise of a Lethal Disease Among Mexican American Hispanic Children,” Obes. Surg., vol. 27, no. 1, pp. 236–244, Jan. 2017. DOI: https://doi.org/10.1007/s11695-016-2440-5
T. Arshad, J. M. Paik, R. Biswas, S. A. Alqahtani, L. Henry, and Z. M. Younossi, “Nonalcoholic Fatty Liver Disease Prevalence Trends Among Adolescents and Young Adults in the 2007‐2016,” Hepatol. Commun., vol. 5, no. 10, pp. 1676–1688, Oct. 2021. DOI: https://doi.org/10.1002/hep4.1760
H. Hagström et al., “Adverse outcomes of pregnancy in women with non-alcoholic fatty liver disease.,” Liver Int., vol. 36, no. 2, pp. 268–74, Feb. 2016. DOI: https://doi.org/10.1111/liv.12902
S. A. Alqahtani and J. M. Schattenberg, “NAFLD in the Elderly,” Clin. Interv. Aging, vol. 16, pp. 1633–1649, Sep. 2021. DOI: https://doi.org/10.2147/CIA.S295524
E. Buzzetti, M. Pinzani, and E. A. Tsochatzis, “The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD).,” Metabolism., vol. 65, no. 8, pp. 1038–48, Aug. 2016. DOI: https://doi.org/10.1016/j.metabol.2015.12.012
D. E. Kleiner et al., “Association of Histologic Disease Activity With Progression of Nonalcoholic Fatty Liver Disease,” JAMA Netw. Open, vol. 2, no. 10, p. e1912565, Oct. 2019. DOI: https://doi.org/10.1001/jamanetworkopen.2019.12565
A. Visekruna and M. Luu, “The Role of Short-Chain Fatty Acids and Bile Acids in Intestinal and Liver Function, Inflammation, and Carcinogenesis,” Front. Cell Dev. Biol., vol. 9, Jul. 2021. DOI: https://doi.org/10.3389/fcell.2021.703218
C. Rives et al., “Oxidative Stress in NAFLD: Role of Nutrients and Food Contaminants,” Biomolecules, vol. 10, no. 12, p. 1702, Dec. 2020. DOI: https://doi.org/10.3390/biom10121702
R. E. Patterson et al., “Lipotoxicity in steatohepatitis occurs despite an increase in tricarboxylic acid cycle activity,” Am. J. Physiol. Metab., vol. 310, no. 7, pp. E484–E494, Apr. 2016. DOI: https://doi.org/10.1152/ajpendo.00492.2015
W. T. Garvey et al., “American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines Formedical Care of Patients with Obesity,” Endocr. Pract., vol. 22, pp. 1–203, Jul. 2016. DOI: https://doi.org/10.4158/EP161365.GL
A. Villani, J. Sultana, J. Doecke, and E. Mantzioris, “Differences in the interpretation of a modernized Mediterranean diet prescribed in intervention studies for the management of type 2 diabetes: how closely does this align with a traditional Mediterranean diet?,” Eur. J. Nutr., vol. 58, no. 4, pp. 1369–1380, Jun. 2019. DOI: https://doi.org/10.1007/s00394-018-1757-3
Y. Ma, K. Chen, L. Lv, S. Wu, and Z. Guo, “Ferulic acid ameliorates nonalcoholic fatty liver disease and modulates the gut microbiota composition in high-fat diet fed ApoE−/− mice,” Biomed. Pharmacother., vol. 113, p. 108753, May 2019. DOI: https://doi.org/10.1016/j.biopha.2019.108753
R. Bernal-Reyes et al., “Consenso mexicano de la enfermedad por hígado graso no alcohólico,” Rev. Gastroenterol. México, vol. 84, no. 1, pp. 69–99, Jan. 2019. DOI: https://doi.org/10.1016/j.rgmx.2018.11.007
S. González, “Dietary Bioactive Compounds and Human Health and Disease,” Nutrients, vol. 12, no. 2, p. 348, Jan. 2020. DOI: https://doi.org/10.3390/nu12020348
Bo’ et al., “Systematic Review on Polyphenol Intake and Health Outcomes: Is there Sufficient Evidence to Define a Health-Promoting Polyphenol-Rich Dietary Pattern?,” Nutrients, vol. 11, no. 6, p. 1355, Jun. 2019. DOI: https://doi.org/10.3390/nu11061355
M. Świderska, M. Maciejczyk, A. Zalewska, J. Pogorzelska, R. Flisiak, and A. Chabowski, “Oxidative stress biomarkers in the serum and plasma of patients with non-alcoholic fatty liver disease (NAFLD). Can plasma AGE be a marker of NAFLD? Oxidative stress biomarkers in NAFLD patients.,” Free Radic. Res., vol. 53, no. 8, pp. 841–850, Aug. 2019. DOI: https://doi.org/10.1080/10715762.2019.1635691
M. Fukaya, Y. Sato, S. Kondo, S. Adachi, F. Yoshizawa, and Y. Sato, “Quercetin enhances fatty acid β-oxidation by inducing lipophagy in AML12 hepatocytes,” Heliyon, vol. 7, no. 6, p. e07324, Jun. 2021. DOI: https://doi.org/10.1016/j.heliyon.2021.e07324
N. M. El-Lakkany et al., “Antifibrotic effects of gallic acid on hepatic stellate cells: In vitro and in vivo mechanistic study,” J. Tradit. Complement. Med., vol. 9, no. 1, pp. 45–53, Jan. 2019. DOI: https://doi.org/10.1016/j.jtcme.2018.01.010
P. Dey, B. D. Olmstead, G. Y. Sasaki, Y. Vodovotz, Z. Yu, and R. S. Bruno, “Epigallocatechin gallate but not catechin prevents nonalcoholic steatohepatitis in mice similar to green tea extract while differentially affecting the gut microbiota,” J. Nutr. Biochem., vol. 84, p. 108455, Oct. 2020. DOI: https://doi.org/10.1016/j.jnutbio.2020.108455
J. Li et al., “Green tea extract protects against hepatic NFκB activation along the gut-liver axis in diet-induced obese mice with nonalcoholic steatohepatitis by reducing endotoxin and TLR4/MyD88 signaling,” J. Nutr. Biochem., vol. 53, pp. 58–65, Mar. 2018. DOI: https://doi.org/10.1016/j.jnutbio.2017.10.016
H.-N. Mu et al., “Caffeic acid prevents non-alcoholic fatty liver disease induced by a high-fat diet through gut microbiota modulation in mice,” Food Res. Int., vol. 143, p. 110240, May 2021. DOI: https://doi.org/10.1016/j.foodres.2021.110240
D. Ivancovsky-Wajcman et al., “Dietary vitamin E and C intake is inversely associated with the severity of nonalcoholic fatty liver disease,” Dig. Liver Dis., vol. 51, no. 12, pp. 1698–1705, Dec. 2019. DOI: https://doi.org/10.1016/j.dld.2019.06.005
Y. Fukuzawa, M. P. Kapoor, K. Yamasaki, T. Okubo, Y. Hotta, and L. R. Juneja, “Effects of green tea catechins on nonalcoholic steatohepatitis (NASH) patients,” J. Funct. Foods, vol. 9, pp. 48–59, Jul. 2014. DOI: https://doi.org/10.1016/j.jff.2014.04.010
U. Hayat, A. A. Siddiqui, H. Okut, S. Afroz, S. Tasleem, and A. Haris, “The effect of coffee consumption on the non-alcoholic fatty liver disease and liver fibrosis: A meta-analysis of 11 epidemiological studies,” Ann. Hepatol., vol. 20, p. 100254, Jan. 2021. DOI: https://doi.org/10.1016/j.aohep.2020.08.071
S. Rafiee, H. Mohammadi, A. Ghavami, E. Sadeghi, Z. Safari, and G. Askari, “Efficacy of resveratrol supplementation in patients with nonalcoholic fatty liver disease: A systematic review and meta-analysis of clinical trials,” Complement. Ther. Clin. Pract., vol. 42, p. 101281, Feb. 2021. DOI: https://doi.org/10.1016/j.ctcp.2020.101281
M. Mazidi, N. Katsiki, and M. Banach, “A higher flavonoid intake is associated with less likelihood of nonalcoholic fatty liver disease: results from a multiethnic study,” J. Nutr. Biochem., vol. 65, pp. 66–71, Mar. 2019. DOI: https://doi.org/10.1016/j.jnutbio.2018.10.001
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 EPISTEMUS

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The magazine acquires the patrimonial rights of the articles only for diffusion without any purpose of profit, without diminishing the own rights of authorship.
The authors are the legitimate owners of the intellectual property rights of their respective articles, and in such quality, by sending their texts they express their desire to collaborate with the Epistemus Magazine, published biannually by the University of Sonora.
Therefore, freely, voluntarily and free of charge, once accepted the article for publication, they give their rights to the University of Sonora for the University of Sonora to edit, publish, distribute and make available through intranets, Internet or CD said work, without any limitation of form or time, as long as it is non-profit and with the express obligation to respect and mention the credit that corresponds to the authors in any use that is made of it.
It is understood that this authorization is not an assignment or transmission of any of your economic rights in favor of the said institution. The University of Sonora guarantees the right to reproduce the contribution by any means in which you are the author, subject to the credit being granted corresponding to the original publication of the contribution in Epistemus.
Unless otherwise indicated, all the contents of the electronic edition are distributed under a license for use and Creative Commons — Attribution-NonCommercial-ShareAlike 4.0 International — (CC BY-NC-SA 4.0) You can consult here the informative version and the legal text of the license. This circumstance must be expressly stated in this way when necessary.
The names and email addresses entered in this journal will be used exclusively for the purposes established in it and will not be provided to third parties or for their use for other purposes.